Building Health: A Physician’s View
Properly Managed IAQ Can Decrease the Spread of Antibiotic Resistance
The role of the indoor environment in shaping health is finally coming into focus.
SCROLL
Documented awareness of the connection between humans, illnesses, and microbes dates to the 1840s, when pediatricians wrote about the role of altered intestinal microbes in children with diarrhea.
Fast-forward to 2012, when the Human Microbiome Project showed that the number of bacteria colonizing our body far out-number human cells. Even more dramatic was the estimate that the microbes living within us contribute 2-20 million genes, compared to our mere 20,000 human genes.1 These facts give a perspective on the human-microbe relationship that is quite different from the germ theory allegation that all microbes are bad. We now know that 95% of identified bacteria are beneficial to our health and support every aspect of being human. As for the other 5%, we need to keep them in check while being mindful that bacteria have been around much longer than humans and have the ability to rapidly pivot as needed to survive in hostile conditions.
The techniques that have revolutionized our understanding of the interplay between human health and microorganisms are genetic analysis tools generally called metagenomics. These allow us to detect the DNA and RNA “fingerprints” of bacterial, fungal, and eukaryotic (e.g., human) cells and viruses living within and among us.
- There are many more bacteria, virus, and fungal types in existence than we previously thought;
- Each of us is an ecosystem with microorganisms living on and within our bodies, and most of these support our health;
- Indoor air compounds, such as particulate matter (PM), ozone, and combustion by-products cause low-grade inflammation in our airways, worsening respiratory infections from pathogenic (disease causing) viruses or bacteria; 2
- Outdoor PM2.5 can carry antibiotic-resistant bacteria (ARB) as well as the gene fragments that carry resistance (ARG), bringing these hazards into our indoor breathing zones;3 and
- The presence of PM2.5, ozone, and nitrogen dioxide indoors or outdoors exacerbate the problem of antibiotic resistance by hastening the transfer of ARG to our naturally occurring respiratory microbes, thus making humans a significant reservoir of antibiotic-resistant genes. 4
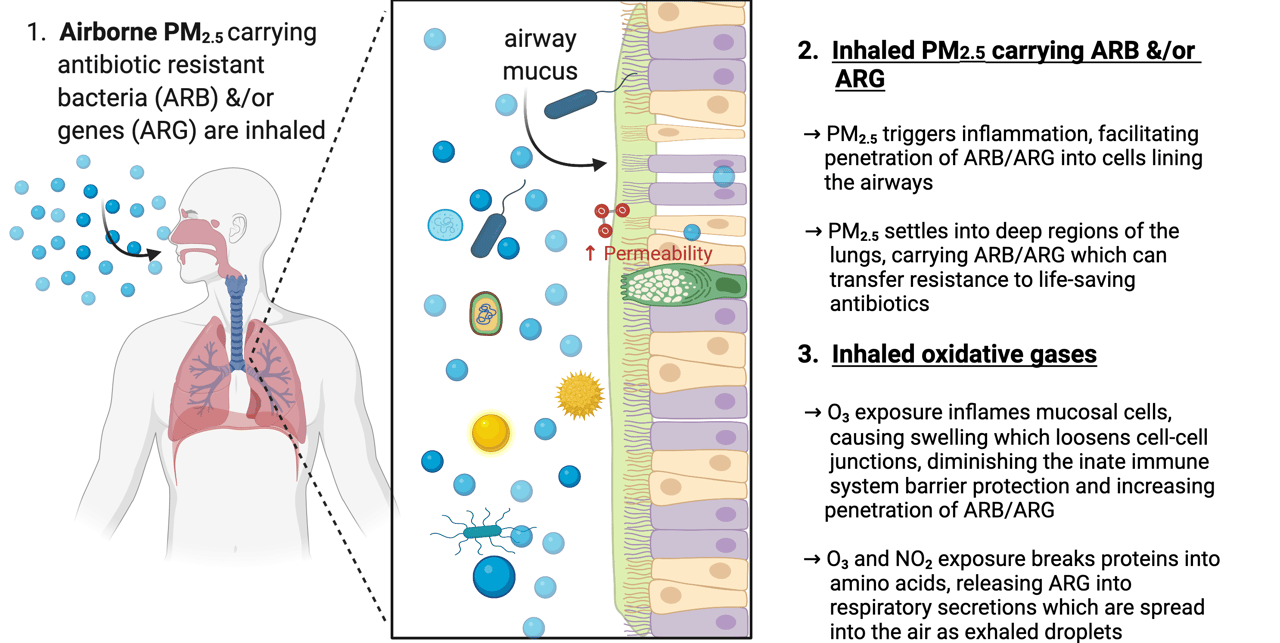
FIGURE 1: The relationship between indoor air pollutants and disease from antibiotic resistant bacteria and genes.
(Figure created via Biorender)
Microbes in the Air
In 2018, many of us were startled by the news that antibiotic-resistant bacteria and genes could spread over long distances through air. 5 Furthermore, the research showed that antibiotic-resistant genes could be passed laterally to other airborne bacteria, immediately conferring resistant to treatment.
We already knew that indiscriminate use of antibiotics had forced the emergence of treatment-resistant bacteria, such as MRSA. Furthermore, we could take some comfort in the logical conclusion that controlling the use of antibiotics would contain and eventually reverse the spread of resistance microbes. Unfortunately, the World Health Organism (WHO) now says otherwise, stating that reducing the use of antibiotics alone will not reverse the trend because of the magnitude of the pool of resistant bacteria and genes that will continue to spread through environmental vectors, such as the air. 6, 6a
So, how can we control the spread of treatment-resistant pathogens?
New findings map bacterial resistance in humans to external sources (waste-water treatment plants, hospitals, animal farms using antibiotics, etc.) from which airborne transmission has occurred. The emission source of resistant microbes can be far away, with ARB and ARG travelling great distances through the atmosphere on fine airborne particles. This pattern, distinct from the spread of resistance through survival pressure following ingestion of antibiotics, has established the key connection between airborne PM2.5 and treatment-resistant pathogens.
Airborne particulate matter not only carries ARB and ARG, but inhalation of PM2.5 also makes the human airway more susceptible to infection. After inhalation, ambient PM2.5 stimulates the transfer of ARGs between the donor bacteria and recipient airway cell through inflammatory changes, such as changes in membrane permeability and alterations in the expression of genes involved in the transfer process. In urban areas with high levels of PM2.5, counts of inhaled ARGs range from 103 to 104 copies/day/adult. 7
In addition to PM2.5, inhalation of oxidative gases, such as O3 and NO2, alter airway cell permeability and protective microbes, increasing the vulnerability of exposed people to respiratory infections from ARB. Ozone also degrades chromosomal polypeptides, releasing free ARG into respiratory secretions and exhaled droplets, so that humans themselves are a source of ARGs and ARB. 8
More research is needed to understand and quantify the role of airborne pollutants in the transmission of antibiotic resistance. Despite the unknowns; however, the critical nature of controlling antibiotic resistance is enough to elevate management of IAQ to the top of our priority list.
The role of the indoor environment in shaping health is finally coming into focus — partly thanks to the COVID-19 pandemic. We are now calling on you, the IAQ professional, because you hold the hope for a better future.
- Annual Review of Genomics and Human Genetics. 13:1, 151-170
- Yang L, Li C and Tang X. 2020. The Impact of PM2.5 on the Host Defense of Respiratory System. Front. Cell Dev. Biol. 8:91. doi: 10.3389/fcell.2020.00091
- Zhu, G., Wang, X., Yang, T. et al. 2021. Air pollution could drive global dissemination of antibiotic resistance genes. ISME J 15, 270–281. https://doi.org/10.1038/s41396-020-00780-2
- Li J, Cao JJ, Zhu YG, Chen QL, Shen FX, Wu Y, et al. 2018. Global survey of antibiotic resistance genes in air. Environ Sci Technol. 52:10975–84
- O’Neill, J. (2016). Tackling drug-resistant infections globally: Final report and recommendations. Review on Antimicrobial Resistance.
- 6.a Merlin, C. (2020). Reducing the consumption of antibiotics: Would that be enough to slow down the dissemination of resistances in the downstream environment? Frontiers in Microbiology, 11, 33. https://doi.org/10.3389/fmicb. 2020.00033
- Xie, Jiawen et. Al. 2019. Bacteria and Antibiotic Resistance Genes (ARGs) in PM2.5 from China: Implications for Human Exposure. Environmental Science and Technology. 53. 963-972. 10.1021/acs.est.8b04630.
- Niu, Y., et.al. 2020. Ozone exposure leads to changes in airway permeability, microbiota and metabolome: A randomised, double-blind, crossover trial. European Respiratory Journal, 56. https://doi.org/10.1183/13993003.001652020
