Building Health: A Physician’s View
Moving Beyond the Wells-Riley Equation
If we're truly going to manage indoor environments for occupant health, we need to extend our understanding and management of IAQ to encompass more than the number of microbes in the air.
SCROLL
IAQ strategies to limit indoor exposure to harmful constituents have been revisited in light of heightened concern about infection control brought on by COVID-19. The goals of these efforts are, understandably, to protect occupants from infectious microbes, such as SARS-CoV-2, that are transmitted through the airborne environment.
A foundational tool to manage airborne viral transmission is the Wells-Riley equation, which was developed in 1974 following an outbreak of measles in an elementary school. Based on the concept of a ‘quantum of infection,’ this model predicts the number of infectious droplet nuclei required to infect 1-1e (i.e., 63.2%) of susceptible persons in an enclosed space.
Almost 50 years later, the model is still valuable in evaluating the efficacy of interventions, such as ventilation, filtration, and humidification, in the removal of infectious respiratory droplets from the breathing zone of potential “secondary hosts” or occupants who could get sick if exposed. While limiting the load of viral particles in the occupant breathing zone is necessary for a safe environment, this is only one of several dynamics that determine the chance of an occupant getting sick from indoor exposures.
If we are truly going to manage indoor environments for occupant health, we need to extend our understanding and management of IAQ to encompass more than the number of microbes in the air. Other key dimensions, shown in Figure 1, include the relationships between IAQ and established building microbial communities (the microbiome), occupant immunity and overall physiological functioning, and conditions passed on to our children through epigenetics.
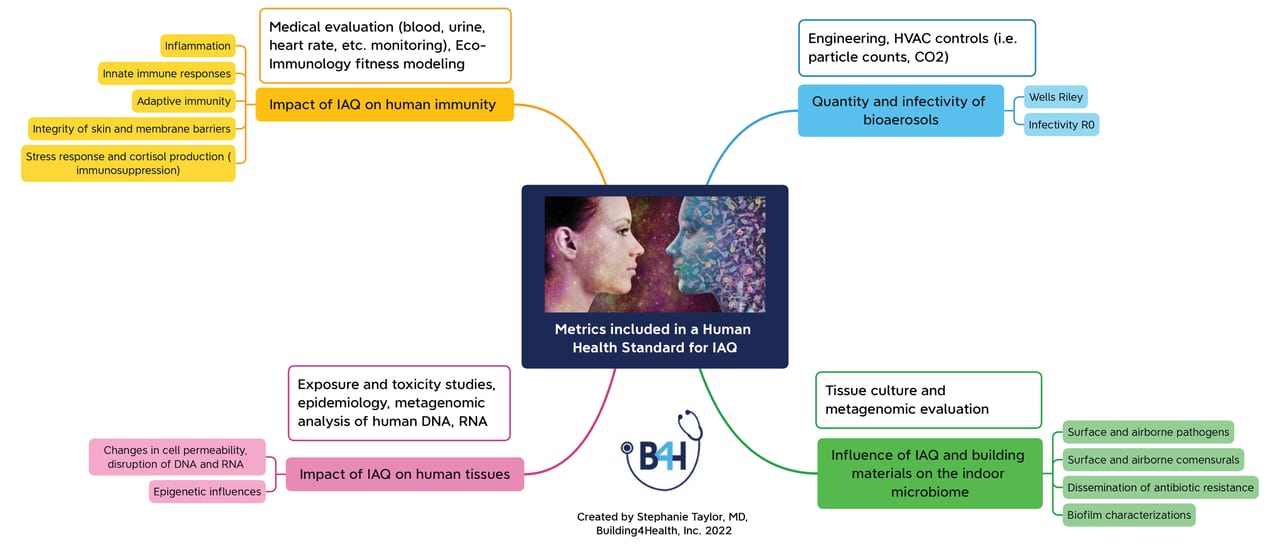
FIGURE 1: The metrics needed for an IAQ human health standard.
Figure courtesy of Building4Health
Balancing Human Cells, Microbes, and Immune Responses
One could argue that reducing exposure to viruses and bacteria should not be the primary focus of IAQ management for health. After all, we are continually surrounded by and innundated with viruses, bacteria, and fungal microorganisms that invade our delicate cell membranes on a regular basis. Every time we brush our teeth, have sex, scratch our skin, or simply inhale, we invite microbes into our bodies through tiny breaches in our physiological barriers. And, yet, when our immune system is functioning properly, these normal behaviors do not result in overwhelming infections. What environmental factors support this homeostasis, allowing our human cells to live in peaceful coexistance with microbes?
We have identified the bacteria and viruses that cause infections, yet the presence of these organisms alone does not predict the full clinical picture of a serious disease. Ironically, the same immunological defenses that prevent the harmful invasion of pathogenic bacteria and viruses can, at times, worsen the clinical outcome of those infections. Without appropriate identification of harmful microbes and regulation of immune-mediated killing, a perverse side effect of these processes can be worsened illness or even the death of the human host. This “friendly-fire” within our bodies can also result in ongoing autoimmune diseases long after the infection has resolved.
To my surprise, there is a field known as eco-immunology, which investigates variations in invertebrate and mammalian immune functions in the setting of changing biotic and abiotic factors. Modeling tools from this fascinating discipline could contribute to our understanding and prediction of the impact of the indoor environment on human immunology and the development of diseases.
Knowing why we get sick and, conversely, why we do not, comes down to a quantitative understanding of the processes responsible for the balance between beneficial microbes, infectious pathogens, human cells, and our immune functioning. Human health and disease, like much in life, are continuous processes occurring within an ecosystem. Let’s harness our motivation to manage indoor environments for health to develop a holistic approach to human-microbe coexistence.